Articulation Coxae
The Cocae Articulation is a spheroidal enarthrose joining the caput ossis femoris with the acetabulum.
The strength in each passing leg element and the strong ligaments make the hip joint a very mobile though dislocatable whole.

The hip joint must be considered in a very narrow relation to this complex anatomical part of the pelvic girdle where an important role is being played.
Because of its construction, there are many consequential possibilities for compensation.
The hip plays a major role during life. On the one hand as a carrier of bodyweight and on the other hand it gives the human being the possibility to automatically move.
 Through this static and dynamic function, the joint
subject to signs of wear and tear, contraction and stretching, gives reactions
upon the ligaments, blood vessels and nerves.
Through this static and dynamic function, the joint
subject to signs of wear and tear, contraction and stretching, gives reactions
upon the ligaments, blood vessels and nerves.
Caput Femoris
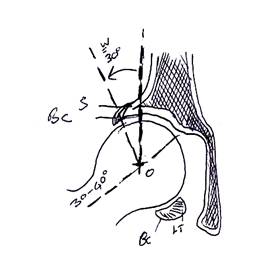
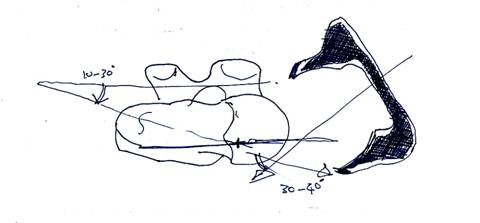
The Caput Femoris is a bowl form. It has an intersection off 4 to 5 cm and is conducted by the Column Femoris. This neck of the femur is connected with the diafysis through the trochantor major and minor. The caput and column are directed above, inwards and to the front, and form an angle from 125 -130° with the diafysis (i.e. the inclination angle).
The caput is 2/3 covered with cartilage except the Fovea Capitus which can be found in the postero-inferio quadrant and is the attaching place of the Ligament Capit Femoris.
 Acetabulum
Acetabulum
Points outward, to the front and under and forms an angle from 30-40° with the horizontal plane and 30-40° with the frontal plane.
It is a half-bowl forming depression at the meeting point from the ilium bone, pubis and ischium.
It comprises of 3 cuttings
- (incisura acetabuli) and a
- moon-forming joint (facies lunata) which is a bordered with the
- deeper lying ruwe holte (fossa acetabuli).
 Around the
acetabulum lies a cartilage-forming ring (labrm acetabulare) which is bridged
over by the incisure ischio-pubicum - thanks to the lig.transversum acetabuli
which joins the ramus anterior actetabulari.
Around the
acetabulum lies a cartilage-forming ring (labrm acetabulare) which is bridged
over by the incisure ischio-pubicum - thanks to the lig.transversum acetabuli
which joins the ramus anterior actetabulari.
Capsula Articularis
The capsula articularis can be found between the coccyx and the proximal end branch of the femur, and consists of:
- Fibrae longitudinales.
- Fibrae oblique.
- Fibrae arcuatae.
- Fibrae circulares.
This has no bone insertion. It forms a zona orbicularis a ring forming band around the neck of the femur.
The capsula attaches to the complete contour of the labrum and on the lig.transversum.
On the femur, it attaches along the linea intra-trochantercia. Behid, it follows along an equidistant line to the crista intra-trochanterica, leaving room for the insertion from M.Obturatorius Internus and the M.Gemelli, M.Obturatorus Externus and M.Piriformis.
Ligaments.
- Lig. Ilio-Femoral.
A strong belt on the fore-side of the capsula-articularis with origin on the ilium (under the anterior inferior iliac spine) and attachment at the linea intra-trochantica).
It is made of two parts:
- An upper bundle: runs to the upper part of the Linea-Intratrochanterica.
- A lower bundle: runs to the lower part of the linea inter-trochantia.
- Ligamentum Pubo-femorale.
This belt runs from the pubic bone (fore-side from the eminentia ilio-pectine over the joint capsule (connecting the zona orbicularis to the femur proximal from trochantor minor).
Both ligaments ilio and pubo femoral form at the foreside the N.Van Welker.
Between lig. Pubo Femorale and lower bundle from the lig. Ilio femoral one can find thhe ilio pectinea bursa over which the psoas runs.
- Ligament Ischio Femoral.
This belt runs from the back brim of the acetabulum over the column to the foreside of the trochanter major and the linea intra-trochantica. It has a connection with the zona obicularis.
During extension, lig. Ilio pubo-femoral as well as ischio femoral become tight whilst during flexion they all relax.
- Ligamentum Capitus Femoris.
Is a flat band in the fossa acetabuli with attachment on the femur in the fovea capitis and attachment on the ilium with 3 bundles:
- A posterior bundle: leaves the acetabulum along the incisure acetabuli (and lig. Transversum) and attaches under and behind the posterior horn of the facies lunata.
- A middle bundle: attaches the upper brim from the Lig.Transversus.
- An anterior bundle: attaching the acetabulum behind the fore-horn of the facies lunata.
The lig. Capitis femoris has no mechanic role as such but is very strong (45kg). Its primary role is to encourage the blood stream (ramus acetabularis).
The bloodsupply from the caput and the column become assured through the arteriae capsulares of the A. Circumflexa femoris mediallis (A. Femoris Profunda, A. Femoralis, A.Iliaca).
Relations of the Articulatio Coxae
- On the Front.
M. Sartorius (from the SIAS to the anserius tendon) divides the frontside into two parts.
a) The region Femoralis Antero-lateralis (trigonum femorle laterale). Between the m. Tensor Fascia lata and M.Sartorios: Trigonum Femoral Laterale.
The triangle exists from the to the bottom:
- The sub-cutaneus tissue with rami n.cutaneus femoris lateralis.
- Aponeurosis (fascia).
- A. and V. profunda femoris.
- The muscles:
o M. Tensor fascia lata (lateral)
o M. Sartorius (medial)
o M. Rectus Femoris. This muscle covers the joint capsule. Proximally, it becomes covered through M.Tensor fascia Lata and M.Sartorius.
b) The region Femoralis Antero-medialis (trigonum femorle mediale van SCARPA). Between the m. Sartorius and m.Adductor Longus: from top to bottom:
o Sub Cutaneus tissue with the V. Saphena Magna and the Nodi Lymphatici inguinale.
o Aponeurosis Femoralis which unfolds in an upper part and a deep layer forming the canalis femoralis (fibrous gaine for the blood vessels running from the lacuna vasorum in the groin until the hiatus saphenus above the knee).
o The muscles m. sartorius, m.adductor longus, m.psoas (lateral), m.pectineus (medial).
- Medial Side
From the upper part to the profound:
- Aponeurosis femoralis.
- M.Gracilis and the medial side of M.Adductor Magnus.
- M.Adductor Brevis.
- M.Obturatorius Externus:
o Origin of the countour from the foramen obturatorium.
o Crossing the underside of the capsule.
o Attachment: Fossa trochanterica.
- Foramen Obturatorium and Membrana obturatoria running through the membrane is the canalis obturatorius which connects the pelvis minor to the anterior-medial side of the thigh.
- Rear Side
Contains from top to bottom:
- The upper level aponeurosis of M.Glueteus Maximus.
- M.Gluteus Medias.
- M.Gluteus Minimus covers the upper side of the articulation.
- The pelvi-trochanter-muscle group:
o M.Piriformis.
o M.Gemellus Sup.
o M.Obturatorius Internus.
o M.Gemellus Inf.
o M.Obturatorius Ext.
o M.Quadratus Femoris covers M.Obturatorius.
- Lateral Side
From the upper area to the deep layer, the hip joint is covered as follows:
- Tractus Ilio-tibialis: an aponeurotic band, along the proximal fusion with the aponeurosis of the M.Gluteus Medius and under along the fascia lata. Along the posterior, it receives the fibres of the M.Gluteus Maximum and along the front from the M.Tensoor Fascia Lata. It attaches to the lateral condyle of the Tibia (tuberculum infracondylare of GERDY).
- The front fibres of the M.Gluteus Maximus.
- The lateral side of the M.Gluteus Medius.
- The front side off the M.Gluteus Minimus.
- The upper and medial side of the Pelvi-Trochanter muscle group.
Blood Supply
The arterial blood supply for the hip:
- A.Circumflexa Femoris Medialis (ramus Profundus) and A.Circumflexa Femoris Lateralis (Ramus Ascendens).
Both are branches of the A. Profunda Femoralis (A.Femoralis, A.Iliaca Ecterna).
They give branches for the Caput and Collumn Femoris.
- Ramus Acetabularis van A. Obturatoria (A.Ililaca Interna)
Runs through the incisura acetabuli together with the Lig. Capitis Femoris and supplies the antero-inferior part of the joint.
- A. Glutea Inferior (A. Iliaca Interna).
Supplies the lower and medial part of the gluteals and the proximal and back part of the thigh.
- Ramus Profundus of A.Glutea Superior.
Supplies the upper part of the joint and gives supply to the ramus acetabularis superior.
Lymph System
Nodi Lymphatica Iliaci Externi
These are grouped around the Vasa Iliaca Externa (above the fold of the groin).
Nodi Lymphatica Iliaci Interni
These are grouped around the Vasa Iliaca Interna.
Nerve Supply
The front branches of the Plexus Lumbalis
N.Femoralis: with the rami musculares before m.pectineus and m.quadriceps.
N.Obturatorius: with branching to the front side of the joint and under and above the pubis.
The rear branches of the Plexus Sacralis
N.Quadratus Femoris with Ramus Gemellus Inferior:
Comes through foramen ischiadicus majus to M.Quadratus Femoris and the hip joint.
BIOMECHANICS
The Hip movement.
- Flexion
Dependent on:
a) The position of the knee:
i. Active - Straight Knee: Hip Extension to 20°
- Bent Knee: Hip Extension to 10°
ii. Passive - Straight Knee: Hip Extension to 30°
- Bent Knee: Hip Extension to 20°
b) The position of the Pelvis: The possibilities of extension become larger by an Anteversion of the pelvis.
Abduction
Becomes restricted with the use of the adductors, through the lig. Pubofemoral and through contact from the column with the border of the acetabulum.
An abduction movement in one hip will be paired with an abduction movement in the other hip.
Also the vertebral column plays a large part in the movement of the hip.
Hip movement amplitude amounts to 15-120°.
Adduction
Restricted by the upper bundle of the lig.iliofemoral.
The amplitude of movement amounts to 30°.
Exorotation
Becomes restricted through the ligaments on the front side of the joint
Amplitude of movement: 60°.
One exerts a exorotation with hip in flexion dan the amplitude of movement is larger, there the lig Bertin is in more tension during flexion.
Endorotation
Becomes restricted through the exorotation and the lig.ischiofemoral. The amplitude of movement amounts to 30-40°.
FUNCTION OF THE HIP LIGAMENTS DURING HIP MOVEMENT
With hip-extension, all ligaments become tense, above all, the lower bundle of the Lig. Ilio Femoral.
From flexion, all ligaments become rellaxded.
From exorotation, all ligaments become tense from the front, above all the upper bundle of lig.iliofemoral and lig. Pubofemoral.
With endorotation, the lig. Ischiofemoral becomes tense, the lig. Pubofemoral and lig.ischiofemoral become relaxed.
With adduction, the upper bundle of the lig.iliofemoral become tense, the lig.pubofemoral and lig.ischiofemoral become relaxed.
During abduction, the lig. Pubofemoral and lig.ischiofemoral become tense, while the upper bundle of the lig. Iliofemoral become relaxed.
Muscle Function
Flexion
M.Iliopsoas, M.Sartorius, M.Rectus Femoris, M.Tensor Fascia Latae, M.Pectineus, M.Adductor longus, M.Gracilis, Front byndles of M.Gluteus Medius and M.Gluteus Minimus.
Extension
M.Gluteus Maximus, M.Semimembranosus, M.Semitendinosus, M.Biceps Femoris, M.Adductor Magnus.
Abduction
M.Gluteus Medius and Minimus, M.Gluteus Maximus (front fibres), M.Tensor Fascia Latae, M.Piriformis, M.Sartorius.
Adduction
M.Adductor Magnus, longus and brevis, M.Gracilis, Hamstrings, M.Gluteus Maximus, M.Quadratus Femoris, M.Pectineus, M.Obturatorius Internus and Externus, M.Gemelli.
Exorotation
M.Piriformis, M.Obturatorius internus and externus, M.Gemelli, M.Iliopsoas, M.Quadratus Femoris, M.Pectineus, The Hamstrings and the rear bundles of M.Glutei (Max, Med, Min).
Endorotation
M.Tensor Fascia Latae, Front Bundles of M.Gluteus Medius and Minimus; M.Iliopsoas. adductors.
Observation of the Hip-joint
The observation of the hip-joint is directed at the possible tracing of the dysfunction of the physiology of the joint
Normal muscle physiology means a balance between muscle length and muscletone.
Problems in this balance (dysfunction) can have as a cause:
- A traumatic or secondary joint dysfunction.
- Chronic or acute pain.
- Visceral problems.
- Radical / Partly radical problems.
- Perifery or central neurological problems.
An harmonic concentrated movement is in this case not longer possible with the different aspects of the muscle function no longer present.
The dysfunction becomes apparent through loss of coordination and by the observation of the elementary movement through loss in amplitude.
This balance system leads to hypertonus or hypotonus.
- Hypertonus: one finds the bending back to muscle-shortening and to a stronger force-development.
- Hypotonus: one finds the beding back to muscle-lengthening and to a weaker muscle; this can lead to real loss of force, but in the first instance this gives loss of coordination.
It is important that the cause of a loss in amplitude can determine:
- if it will be a muscle problem.
- If it will be a joint problem.
- If it will be a neurological (central/peripheral) problem.
For this to determent, the cause always has an effect bilaterally, where a loss in amplitude is the cause, the cause my give hypertonus on one side, and hypotonus on the other side.
DIAGNOSTIC OF THE HIP-JOINT
The diagnostic of a hip-joint is supported by the following test procedures:
- Amplitude test.
This is a passive test. It is an assessment and comparison of the muscle length.
The therapist asks the required softness and a very fine kinetic feeling.
In the measure that the smallest muscle tension can be noted.
The different possibilities of amplitude test:
a) The amplitude is the same on both sides. This means a balance in muscle function.
b) The amplitudes is different. This means a problem from the balance in muscle function.
- Force test.
This is an active test. For this dysfunction to be determined, the force test should be used in combination with the results of the amplitude test.
The different possibilities of the force test are:
a) Force is the same on both sides. In this case, thhe hypertone or the shorter side should be treated with muscle energy technique. i.e. search for the motoric barrier, 6 x contraction, relax, win in the amplitude.
b) There is a difference in force. In this case, the weaker side (the larger amplitude side) should be treated with iso-kinetic contractions.
The repeat of contraction increases the activity in the muscle bundles and sets the muscle in a beter response given by the force test.
c) There is a difference in force but on the side of loss of amplitude it is weaker. In this case, it is not a muscular cause, rather an articular or neurological cause.
TERMINOLOGY
Loss of extension = Dysfunction in Flexion.
Loss of abduction = Dysfunction in Adduction.
Loss of exorotation = Dysfunction in Endorotation.
MUSCLE TESTS
Hamstrings
The test is done with a straight knee.
Amplitude Test.
P. On the back.
O. Hold each leg tot the motoric barrier and compares the both amplitudes.
The motoric barrier becomes assessed when the observer feels the muscle tension and the knee bending presents a flexion or when the pelvis begins to move.
Force Test.
P. On front. Knees bent 30-60-90°.
O. Asks the patient to make a knee-flexion against resistence.
Abductors
Here, the adduction is tested.
Amplitude Test.
P. On the back.
O. Performs a maximal adduction and compares bilaterally.
The maximum adduction is assessed when the observer feels tension in the muscle or when the pelvis begins to move.
Force Test.
P. On the back. Tries to do abduction movement against resistence.
O. Compares bilaterally.
Adductors.
Here, the abduction is tested.
Amplitude Test.
P. On he back.
O. Stands next to the patient or at the foot end. He takes the leg of the patient at the ankle and performs an abduction movement. The pelvis should not move. Execute bilaterally and compare.
Force Test.
P. On the back.
O. The leg to be tested from the abduction position. The patient adducts bilaterally against resistence which is compared.
The Endo-Rotators.
Exorotation is tested.
Amplitude Test.
P. On the front, knees 90° bent.
O. Stands at the foot end and executes a bilateral exorotation.
Force Test.
P. On the front, knees 90° bent.
O. Stands at the foot end of the patient. Performs an exorotation. The patient edorotates against resistance this is then compared.
Exorotators
The endorotation is tested.
Amplitude Test.
P. On the front, knees 90° bent.
O. Performs an endorotation.
Force Test.
P. On the front, knees 90° bent.
O. Stands at the foot end of the patient. Patient exorotates against resistence. This compared.
Flexors
The extension is tested.
Amplitude Test.
P. On the front.
O. Cranial hand fixes the pelvis. Straightened leg is held (before the M.Psoas) or bent knee is held (before the M.Rectus femoris).
Variation. Patient lying on the back at the end of the table with one leg in the knee-thorax holding. The leg to test hangs under. Compare bilaterally.
Force Test.
P. On the front.
O. Takes the leg of the patient in cradle holding and asks him to push the leg against the table (m.psoas). Bilaterally execute and compare.
Variation 1. Patient lies on the back with bent knees, lower leg outside the table.
Observer stands between the knees of the patient and asks him to perform a hip flexion against resistence (compare bilaterally m.psoas).
Variation 2. On the front with bent knees. Observer sits at the foot end of the table and holds both ankles on his shoulders. He asks the patient to perform a bilateral extension against resistance.
TREATMENT OF HYPERTONUS and HYPOTONUS.
Hypotonus can be treated with iso-kinetic contractions. The patient is asked to contract the agonist. The repeat of the contraction increases the possibility of stimulation through more muscle bundles becoming activated.
Hypertonus is treated with the Muscle Energy technique i.e. search for the motoric barriere, contraction, relax and win in amplitude.
Hypotonus of the abductors.
P. On The side.
O.. At the front of the patient. The cranial hand on the crista iliaca, the caudal hand takes the ankle. He asks the patient to perform an iso-kinetic contraction.
Hypertonus of the abductors.
P. On the back.
O. At the foot end or at the dysfunction side of the patient. Brings the leg in dysfunction into adduction and lies his hand on the other knee, the leg resting on the arm of the observer.
Search for the motoric barrier, isometric contraction, relax and win.
Hypotonus of the adductors.
P. On the back.
O. Sits between the legs of the pation with his back to the unaffected leg in order to stabilize it. The affected leg is brought into abduction. Iso-kinetic method.
Hypertonus of the adductors.
P. On the back.
O. Stands between the legs of the patient and brings the leg into abduction to the motoric barrier. Kontact, relax and win.
Hypotonus of the Endorotators.
P. On the front, knee 90° flexion.
O. Stands at the affected side and fixes the pelvis. Brings the leg in exorotation (motoric barrier). Isokinetic method.
Hypertonus of the Endorotators.
P. On the front, knee 90° flexion.
O. Stands at the affected side and fixes the pelvis. Brings the leg into exorotation (motoric barrier). Myotensive method.
Hypotonus of the Exorotators.
Same as for endorotator.
The leg goes into endorotation to the motoric barrier, isokinetec methid.
Hypertonus of the Exorotators.
Same idea as for the edorotators. (only the leg now goes into to endorotation for the motoric barrier).
Hypotonus of the Flexors
P. On the back, the affected leg hanging over the table edge, the other is bent and fixed itself against the table or observer.
O. Stands on the side or at the foot end of the patient and brings the hip to extension (motoric barrier).
With isokinetic method, he asks for hip-flexion against resistence.
Hypertonus of the Flexors
Same holding as for hypotonus. Isometric method.
EXCLUSION TESTS
Exclusion Test between a Sacro-Iliac and Coxo-Femoral Dysfunction.
P. Lying on the back. Legs bent at 90° (knee-thorax holding).
O. Stands at the dysfunction side. Straightens the affected leg up to the point where the symptoms appear. At this point, he fixes this holding and with the other hand, he puts pressure on the superior anterior iliac spine at the same side.
!! When the symptoms reduce this is a sacro-ilac dysfunction.
!! When the symptoms increase - this is a coxo-femoral dysfunction.
Exclusion Test between a Sacro-Iliac and Lumbar Dysfunction.
P. On the front.
O. Thumbs push vertically from both sides of the processus spinosus of S1.
!! Decrease in pain Dysfunction L5-S1.
Exclusion Test between Sacro-Iliac and a Discus Pathology.
P. On the back, legs straight.
O. Holds the leg to the symptoms of the ischial region.
!! With an ischias problem from a discal origin, the Lassθgue signs shall increase with dorsal flexion of the foot.
!! With a sacro-iliac dysfunction, this is not the case, but the symptoms may well appear with the holding of the other leg with dorsal flexion of the foot.
Dysfunction Mechanism
|
DYSFUNCITON |
Movement Restriction |
Muscle |
Ligaments |
Result from Primary Dysfunction during Shortening |
Result from Secondary Dysfunction during Lengthening |
|
EXO |
ENDO |
M.Piriformis M.Obt. Internus. |
Ischiofemoral |
M.Piriformis M.Obt.Int |
Shorter Leg Ilium Ant. Outflare Sacrum Post R/L L/R. |
|
ENDO |
EXO |
m. TFL m. Glut. Min. Adductors |
Iliofemoral Pubofemoral |
m. TFL m. Glut Min. Adductors |
Longer Leg Ilium Post. Inflare. Sacrum Ant L/L R/R |
|
ABD |
ADD |
m. Glut Med. m. TFL |
Iliofemoral |
m.Glut Med. M. TFL |
Inflare (TFL) Ilium Ant. (m.Glut Med). |
|
ADD |
ABD |
Adductors |
Pubofemoral Ischiofemroal |
Adductors |
Adductors Pubis Sup. |
|
FLEX |
EXT |
m. Psoas m. Iliacus |
Iliofemoral Pubofemoral Ischiofemoral |
m.psoas m.iliacus |
Lumbal compensation. Visceral problem. |
|
POSTERIORITY |
Variying production. EXO+++ |
Varying production. Smaller leg and ENDO Caput post. |
Capitis Femoris. Pars Posterior |
|
Ilium Post. Inflare. |
|
ANTERIORITY |
Varying Production. ENDO+++ |
Varying production. Longer leg and EXO. Caput ant. |
Capitis Femoris. Pars Anterior |
|
Ilium Ant. Outflare.
|
Secondary Dysfunction of the Art.Coxae:
- M.Psoas: - Colon Ascendens.
- Colon Descendens.
- Fascia Iliacus (kidney).
- M.Iliacus: - Caecum.
- Sigmoid.